침은 어떤 기전으로 염증을 완화시키는가
다리 부위 혈위 #전침자극으로 어떻게 위험하고 치명적인 #패혈증 sepsis의 치료가 가능한가
미주신경-부신 축을 구동하는 전침의 신경해부학적 기초
미국 하버드대학 신경생물학 Ma Qiufu 교수팀은 Prokr2 단백의 감각신경원에서 해답을 찾았다
Abstract
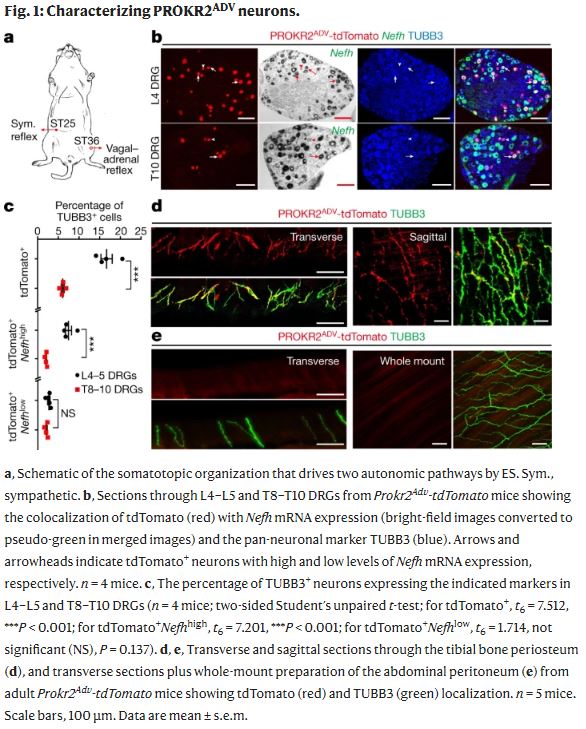
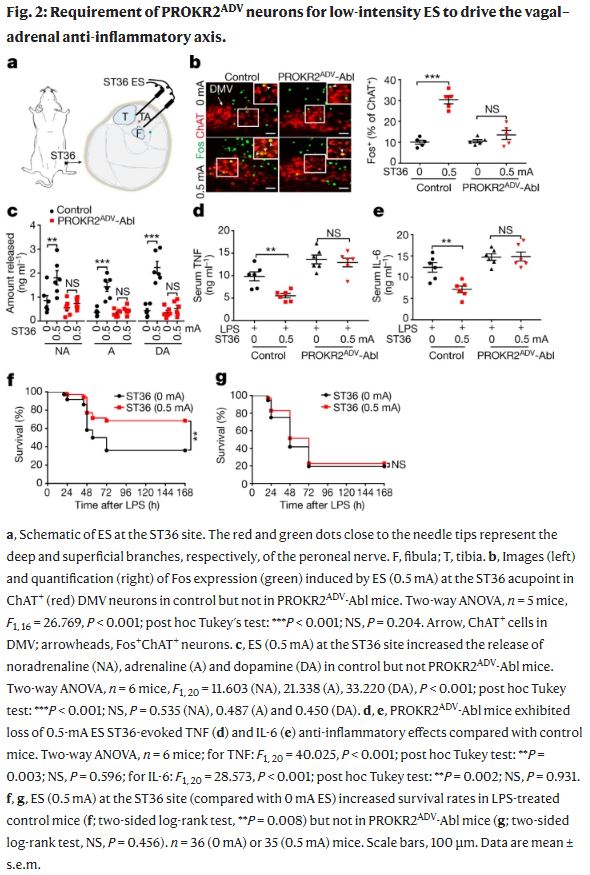
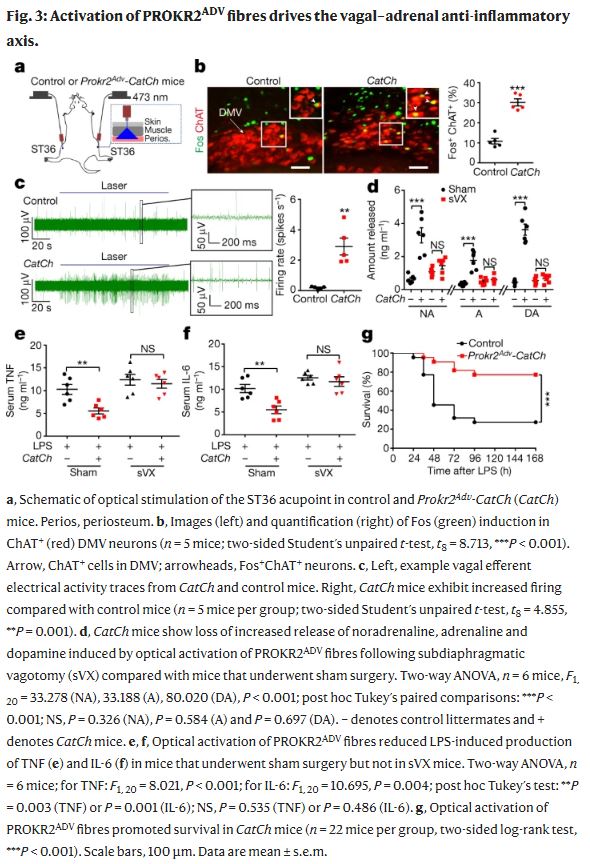
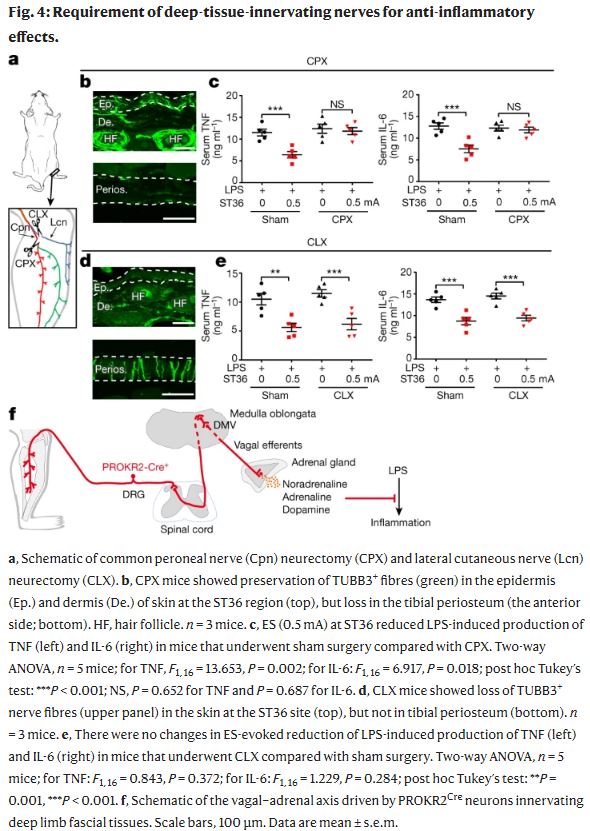
Somatosensory autonomic reflexes allow electroacupuncture stimulation (ES) to modulate body physiology at distant sites1,2,3,4,5,6 (for example, suppressing severe systemic inflammation6,7,8,9). Since the 1970s, an emerging organizational rule about these reflexes has been the presence of body-region specificity1,2,3,4,5,6. For example, ES at the hindlimb ST36 acupoint but not the abdominal ST25 acupoint can drive the vagal–adrenal anti-inflammatory axis in mice10,11. The neuroanatomical basis of this somatotopic organization is, however, unknown. Here we show that PROKR2Cre-marked sensory neurons, which innervate the deep hindlimb fascia (for example, the periosteum) but not abdominal fascia (for example, the peritoneum), are crucial for driving the vagal–adrenal axis. Low-intensity ES at the ST36 site in mice with ablated PROKR2Cre-marked sensory neurons failed to activate hindbrain vagal efferent neurons or to drive catecholamine release from adrenal glands. As a result, ES no longer suppressed systemic inflammation induced by bacterial endotoxins. By contrast, spinal sympathetic reflexes evoked by high-intensity ES at both ST25 and ST36 sites were unaffected. We also show that optogenetic stimulation of PROKR2Cre-marked nerve terminals through the ST36 site is sufficient to drive the vagal–adrenal axis but not sympathetic reflexes. Furthermore, the distribution patterns of PROKR2Cre nerve fibres can retrospectively predict body regions at which low-intensity ES will or will not effectively produce anti-inflammatory effects. Our studies provide a neuroanatomical basis for the selectivity and specificity of acupoints in driving specific autonomic pathways.